The problem of joint diseases is always relevant. After forty years, about a third of all people begin to feel pain during movement, and after fifty more than half of the population begins to feel pain. The gradual destruction of the cartilage, ligaments, bones and soft tissues around the joints is referred to by doctors by the general term "osteoarthritis".
How can this condition be prevented? And what treatments will help relieve pain when the disease has already developed? To answer these questions, you must first understand the difference between arthritis and osteoarthritis, the most common joint diseases.
What is arthritis?
What is the main difference between arthritis and arthrosis can be understood from the names: acute and sudden diseases end with "-itis"; with "-da" – diseases with a slow course, chronic processes.
Arthritis is an inflammatory lesion of the joints that occurs due to a malfunction of the immune system due to infections (for example strep throat or otitis media), trauma, metabolic disorders, hypothermia, stress or other reasons (including autoimmune).
The first signs look like this:
- sharp pain in one or more joints (often not only during movement), especially early in the morning;
- enlargement, swelling, edema, redness of the painful joint;
- a noticeable increase in temperature at the site of inflammation.
Inflammatory processes caused by arthritis can affect the entire body. In this case, the patient feels high fever, chills, loses strength and may experience inflammation of other organs (eyes, genitourinary system, even heart, lungs, liver and kidneys).
Arthritis has several dozen forms. The most common are:
- rheumatism– inflammation of the connective tissue of large and medium-sized joints that occurs after infections;
- rheumatoid arthritis– a slow autoimmune process that symmetrically affects multiple joints at the same time; causes the appearance of "nodules", pain, loss of mobility; can cause inflammation of many organs;
- gout– caused by the accumulation of uric acid in the blood and salts in the joints; most often it begins with a sharp pain in the big toe joint;
- reactive arthritis– occurs against the background of damage to the body caused by infections (chlamydia, streptococci, etc. );
- infectious arthritis– begins due to a bacterial infection of the joint itself.
What is osteoarthritis?
Unlike arthritis, arthrosis is not accompanied by inflammatory processes. It causes poor circulation in the joint, which causes dryness of the cartilaginous parts.
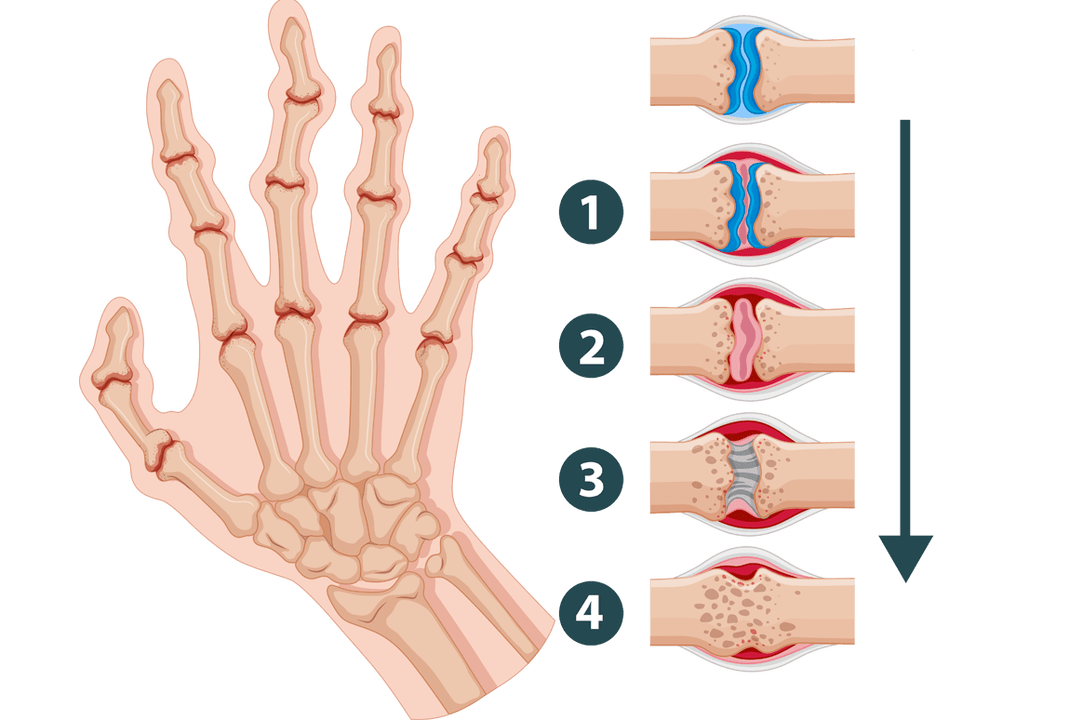
Osteoarthritis is a disease that deforms and destroys joint tissue. With it the connecting layers dehydrate, become thinner and "worn out". The bones begin to touch each other, which causes pain and makes it difficult for a person to move.
Signs of arthrosis of the joints are:
- after a long period of immobility (for example night rest), the joint "freezes", but then develops rapidly when activity resumes;
- the functioning of the joint is accompanied by strange sounds (clicking, creaking, screeching);
- physical activity causes pain.
What are the differences between arthritis and arthrosis?
Both of these diseases affect the joints. But they are caused by different reasons, proceed differently and can lead to very different consequences. Only a correct diagnosis, based on the difference between arthritis and arthrosis, can prevent irreparable damage to the body.
It takes time for cartilage tissue degeneration to develop sufficiently and bone deformation to begin. Therefore, chronic arthrosis usually manifests itself at an advanced age (after 60, less often after 50). The most sensitive to changes are the joints that constantly work under load: the fingers of musicians, the knees of athletes and loaders, the ankles of people who walk a lot or work while standing, etc.
Conversely, arthritis can also occur in a child. The inflammatory process causes pathology of the synovial membrane, saturated with blood vessels, and joint fluid (while in arthrosis it is simply produced in insufficient quantities). Unfortunately, nearly one in five cases of disability worldwide is caused by various forms and complications of arthritis.
Inflammation can affect not only joints, but also other tissues with active blood circulation: blood vessels and heart, lungs, abdominal organs, eyes, urinary system, etc. On the other hand, arthrosis is limited by local mechanical damage to bones and the formation of osteophytes in areas of joint deformation. Although in late stages and advanced forms, the disease can also lead to disability, completely immobilizing a person's limbs.
How do arthritis and arthrosis manifest themselves?

Let's compare the external manifestations to clearly explain the difference between the symptoms of arthritis and arthrosis.
- Ache. In the initial stages of osteoarthritis (which lasts for years), joint pain occurs during physical activity and disappears after rest. It is rarely sharp and loud. Even during the development of the disease, when pain can appear even with small movements and even at rest, it is usually enough to give the body a comfortable position for the pain to decrease. With arthritis, the patient is disturbed by attacks of acute pain of great strength, which can only be extinguished with special drugs. A characteristic symptom is pain during rest, especially early in the morning.
- Clicking, grinding, creaking of the joints. In joints affected by arthrosis, the cartilaginous layers are destroyed. They stop protecting the heads of the bones from contact with each other. Therefore, when they move, the bones touch and rub, producing rough, dry sounds. The more the disease progresses, the louder and louder the clicking in the joints. Arthritis is usually not accompanied by such symptoms.
- Deformation of the joint and surrounding tissues. The development of arthrosis over time causes a change in the shape of the bones: their heads begin to crumble and wear out, and osteophytes may appear. Sometimes swelling and aching pain occur in acute stages, but these symptoms are not permanent. But a joint affected by arthritis becomes inflamed and swollen. Forms of swelling and compaction occur. The skin turns red and becomes hot.
- Limited mobility. Osteoarthritis causes stiffness in a specific joint that disappears with movement. In deeper stages, stiffness increases, flexion amplitude decreases, ultimately leading to immobility. With arthritis, you may feel stiff throughout your body, and attempts to move will cause sharp pain.
- Changes in blood composition. Osteoarthritis is not an inflammatory disease, so it is not reflected in the analysis. Arthritis causes a significant increase in erythrocyte sedimentation rate, which indicates an active infectious and inflammatory process.
Therefore, symptoms of osteoarthritis in the early stages can rarely cause severe anxiety and discomfort. This leads to a negligent attitude and late diagnosis of the disease, which means it complicates further treatment.
Causes of osteoarthritis
There are several factors that increase the risk of pathological changes in the joints and surrounding tissues: constant overload, imbalance of the immune and hormonal systems, poor physical fitness. Therefore, to prevent diseases, you need to regularly follow these recommendations:
- Maintain moderate physical activity through simple exercises, walking, swimming, etc. This will help you get rid of excess weight, improve blood circulation, strengthen muscles and thus relieve stress on the joints.
- Try to eat healthy foods. Fatty foods, red meat and alcohol can be harmful. On the contrary, seafood, fruits and vegetables, dishes containing cartilage and gelatin will be beneficial for the body. It is important to drink plenty of clean water (2-3 liters per day).
- Choose suitable clothes and shoes: comfortable, warm enough heels that do not restrict movement.
- If possible, avoid stress, interruptions and other "shocks" to the body.
However, if a person has already been diagnosed with arthritis or arthrosis, before performing even such simple actions, it is necessary to consult a doctor. In some cases, even conventional prevention can cause harm and worsen the condition.
But how are arthritis and arthrosis treated? What is the difference? The causes of these pathologies differ: immune processes, fight against infections in the first case versus malnutrition of the cartilage in the second. Therefore, the ways of dealing with them will be different. To choose the right course of action, you must first make an accurate diagnosis.
To do this, it is best to undergo x-ray and MRI in combination with laboratory tests of blood and urine. After studying the results, the doctor will prescribe appropriate recommendations.
Arthritis treatment
If the acute form of the disease is caused by an infection, it can be treated with antibiotics. But in this case it is important to accurately select the drug: it is necessary to neutralize the pathogenic bacteria before the joint pathology becomes irreversible. The course is supplemented with anti-inflammatory and immune support drugs.
In case of chronic arthritis (e. g. rheumatoid), treatment must be carried out regularly throughout life. The most commonly used are corticosteroids, cytostatics and modern biologics. These are quite powerful drugs, so to ensure that they do not cause harm to the body, the correct calculation of dosages, frequency and duration of use is essential.
In case of severe pain, the doctor may also prescribe a course of analgesics. And concomitant support methods are necessarily recommended: diet, physiotherapy and a course of physiotherapy. If the inflammation has spread to other organs, the patient must undergo further specialist examinations.
Treatment of osteoarthritis
Modern methods make it possible to almost completely eliminate the manifestations of the disease if the diagnosis was made at an early stage and the patient's age does not reach forty years. To do this, in addition to standard monitoring of stress on the joint and a course of drugs (they start regeneration, restore nutrition and hydration of the cartilage), the patient can be prescribed mud compresses, electrophoresis and acoustic therapy (which affects the affected tissue with low frequency sounds).
In elderly people or in advanced forms, arthrosis cannot be completely cured, although it is possible to achieve a significant improvement in the condition and slow down the destructive processes of the joint. This requires strict adherence to the doctor's recommendations: regular use of medications (for example, chondroprotectors), maintaining a healthy lifestyle, timely completion of prescribed procedures, monitoring joint load.
In arthrosis, the main attention is paid to the restoration of the cartilaginous layer. If concomitant symptoms of inflammatory processes are present, antibiotics or corticosteroids may be prescribed to relieve the acute phase and switch to the main therapeutic regimen. In some severe cases, surgery and even the implantation of an artificial joint may be necessary.

























